- Navigator
- Expansion Solutions
- Industry Analytics and Strategy
- Workforce Development
- Healthcare and Social Assistance
 This article was originally published in the November/December 2022 issue of Expansion Solutions Magazine.
This article was originally published in the November/December 2022 issue of Expansion Solutions Magazine.
While most all industries and related jobs have been impacted by COVID-19, healthcare has been impacted more than most. Healthcare is impacted by the same dynamics that face other industries and the economy including supply chain constraints, workforce shortages, and rising costs but also profoundly impacted by being on the frontlines of critical care, diagnostics and testing, and related services. So how is the healthcare industry responding and performing? What challenges remain and are constraining the industry? What opportunities are on the horizon? The following is an overview of latest trends in the healthcare industry and a specific look at the workforce opportunities and challenges. In the end, it is meant to be an imperative for a focus on workforce development in healthcare.
The healthcare sector is one of the most significant sectors of the US Economy. In 2022 it consisted of more than three million businesses, 23. 9 million workers, and generated more than 3.3 trillion in revenues. Whether rural or urban, north, or south, east or west, or anywhere in between communities and regions have an economy reliant on the healthcare industry for employment, real estate demand, business-to-business purchases, and more.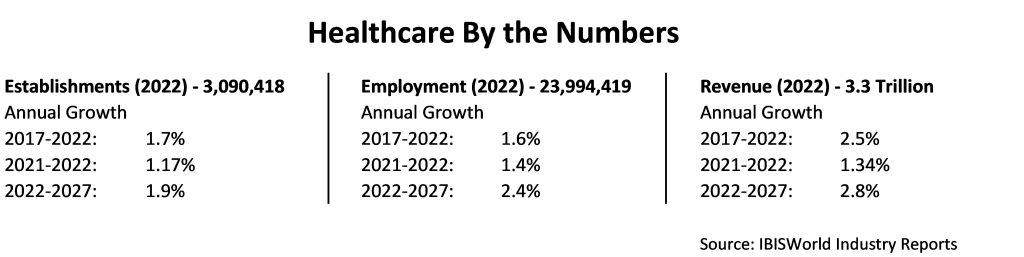
Industry Trends
Multiple factors are impacting the economic trends and outlook for healthcare. COVID-19 is top of mind when assessing healthcare trends, challenges, and outlook. COVID-19 simultaneously put enormous strain in demand on major parts of the healthcare system particularly hospital and emergency care, while also significantly restricting demand due to closures for specialty and short-term, non-essential services. It also placed significant strain on the supply chain most notably for respiratory devices, test kits, personal protection equipment, but much more. Many of these factors have begun to recover and will likely recover fully over the course of the next few years. However, one factor has had a profound impact on healthcare and will likely take many years to recover, and that is workforce. Attracting and retaining workers and providing workforce development to meet needed skills and qualifications was mounting as a major threat to economic growth prior to COVID-19 across all industries. This was driven by many factors including aging population, constraints on immigration, rapid technological change, wage increases not keeping pace with profits, and more. COVID-19 exacerbated the problem by creating significant stress and burnout in the workforce.
When taking into consideration the challenges healthcare faces as an industry it has and is projected to be a growth industry. From 2017 to 2022 healthcare grew at an annual rate of 1.6% in terms of employment and 2.5% in terms of revenue. Looking ahead to 2027, healthcare is projected to grow at an annual rate of 2.4% in employment and 2.8% in revenue[1]. One of the factors contributing to this growth is the increase in federal funding for Medicare and Medicaid. During this period funding grew at an annual rate of 4.4% and in 2022 fees and reimbursements from Medicare and Medicaid represented the second-largest source of revenue or 26.2% of revenue, for the healthcare industry[2].
A healthcare service method that was growing prior to COVID-19 but has since been experiencing accelerated growth is the digitization of healthcare and telehealth. “Of note, while many health plans provided coverage for telemedicine in some capacity prior to the pandemic, few enrollees utilized this service. However, in the five-month period of March 2020 to August 2020, the share of outpatient visits received via telehealth increased to 13.0%, according to a report by the Kaiser Family Foundation and the Peterson Center on Healthcare[3]. And, while some of the use of telemedicine has receded as in-person visits have increased post-pandemic, the overall level is higher than in the past and the use will continue to grow. This will be driven by both technology and convenience, but also by the need for healthcare systems to create efficiencies and control costs. This is already being experienced by use and adoption by healthcare systems and their insurance providers. An area that has grown particularly rapidly is use of social and mental health services.
Healthcare Industry Trends by Subsector
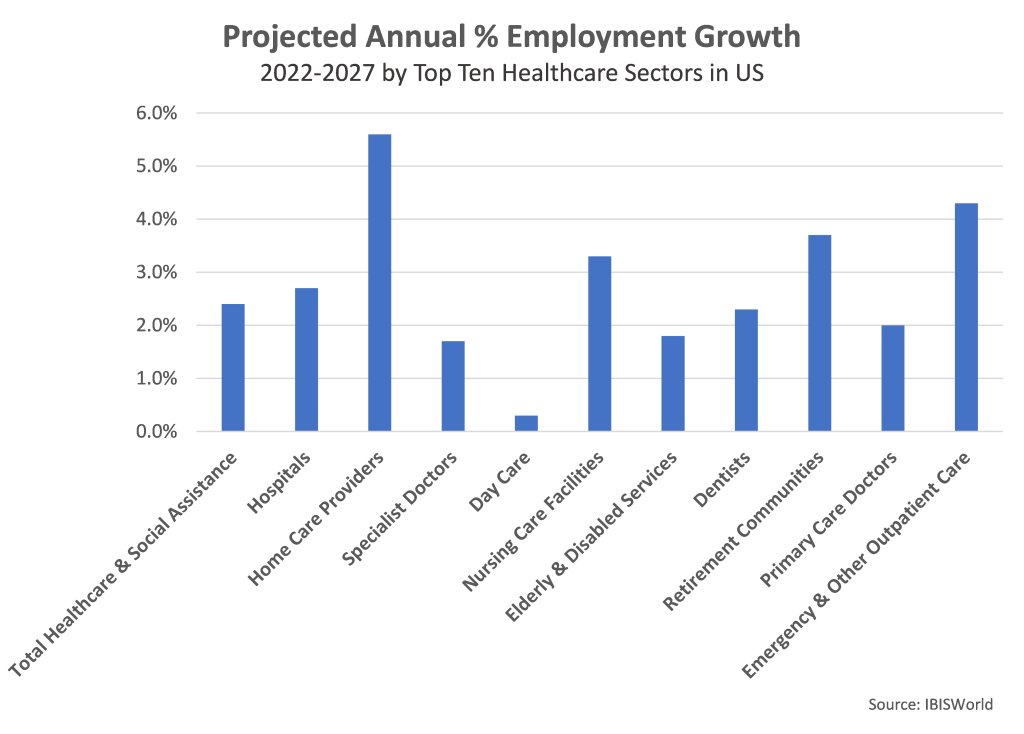
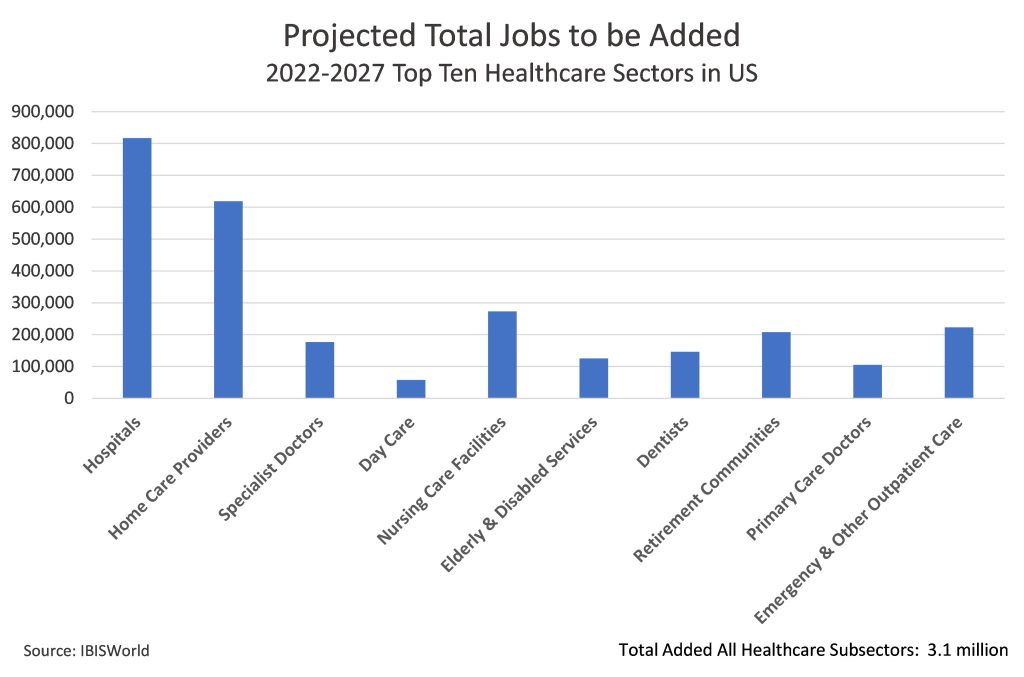
In terms of specific healthcare industry subsectors in the US, hospitals are by far the largest with 5.8 million employees in 2022. A large and rapidly growing subsector is home care providers which in 2022 was the second largest subsector with more than two million employees. It is also projected to be the fasted growing among the top ten largest subsectors with a projected annual growth rate of 5.6%. The increasing demand for care for the aging population is also evident in the data beyond home health services with nursing care facilities and retirement communities all in the top ten largest subsectors and along with home health projected to grow at a rate faster than healthcare overall through 2027.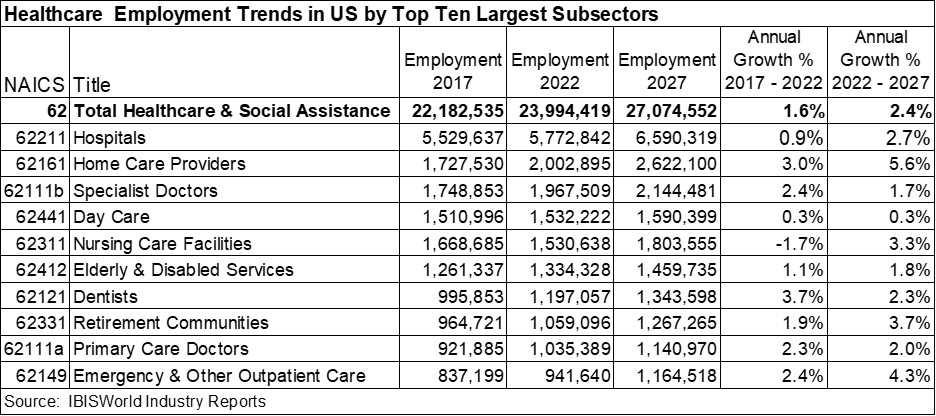
Workforce Challenges and Opportunities
Attracting and retaining workers and providing workforce development to meet needed skills and qualifications was mounting as a major threat to healthcare sustainability and growth prior to COVID-19 and will continue to have a profound impact on the industry for many years to come.
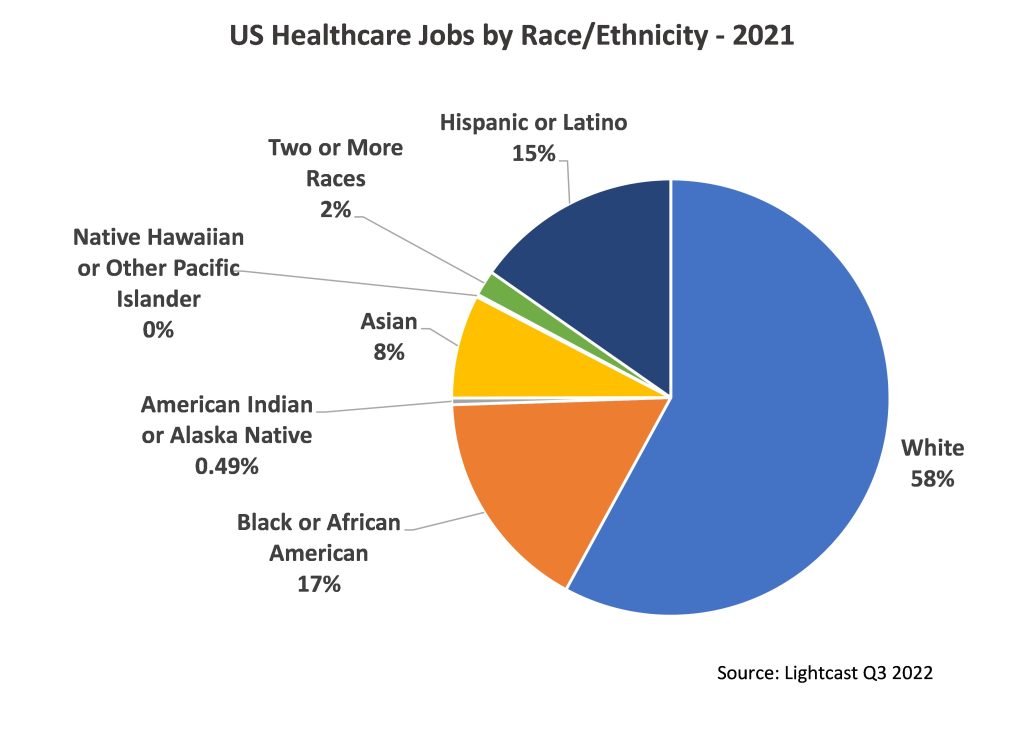
Healthcare has a diverse set of occupations, careers, and workers that fill them. Based on 2021 data 77.8% of the healthcare workforce is female and 22.2% is non-white in terms of race or ethnicity.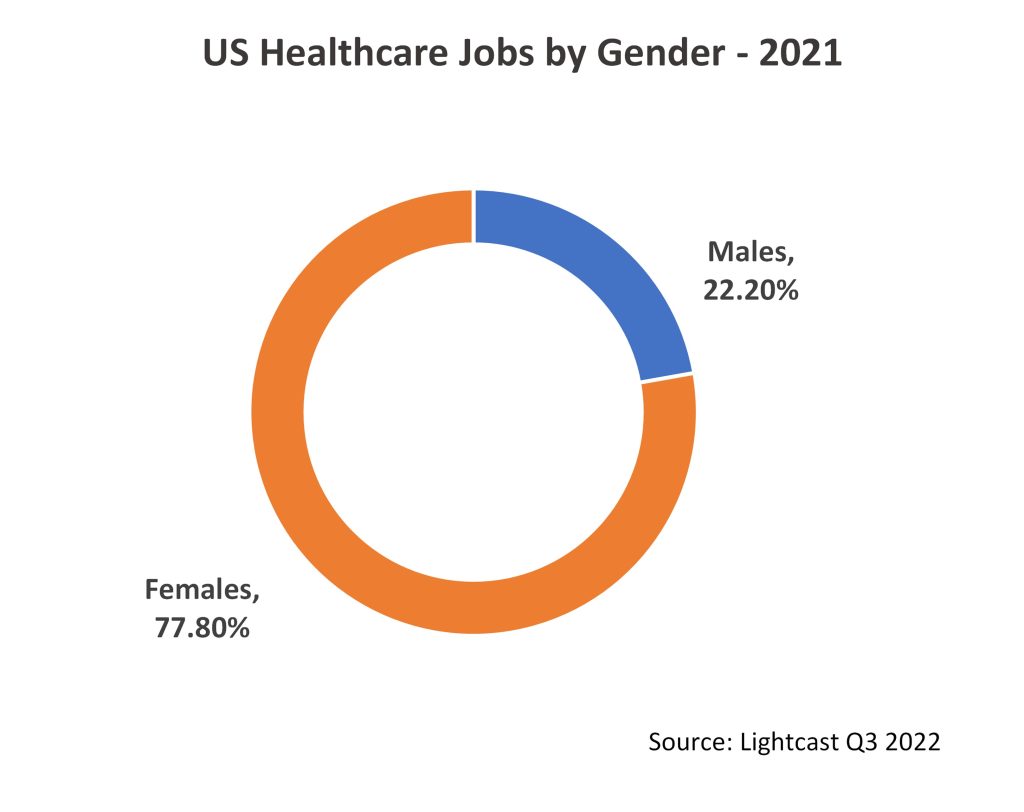
 Jobs in healthcare range from doctors and nurses to aides and assistants to janitors and food preparation and beyond.
Jobs in healthcare range from doctors and nurses to aides and assistants to janitors and food preparation and beyond.
Home Health & Personal Care Aides, Registered Nurses, Nursing Assistants, and Medical Assistants account for 36.2% of the jobs, 7.6 million jobs in 2021. All except nursing assistants grew between 2016-2021 and all are projected to grow considerably through 2026. Together they are projected to add 874 thousand jobs by 2026.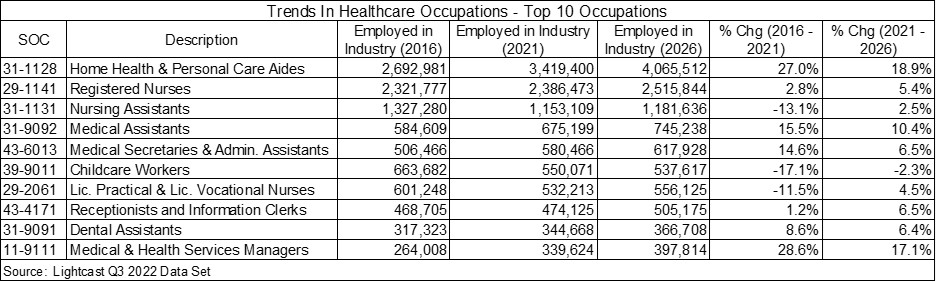 Of all the jobs in healthcare in 2021, 65.9% do not require a bachelor’s degree or higher, and these jobs are projected to grow by 8% through 2026. Of the top ten occupations in 2021, only two — registered nurses and medical and health services managers — typically require a bachelor’s degree or more. This indicates that healthcare occupations are very attainable for large portions of the workforce.
Of all the jobs in healthcare in 2021, 65.9% do not require a bachelor’s degree or higher, and these jobs are projected to grow by 8% through 2026. Of the top ten occupations in 2021, only two — registered nurses and medical and health services managers — typically require a bachelor’s degree or more. This indicates that healthcare occupations are very attainable for large portions of the workforce.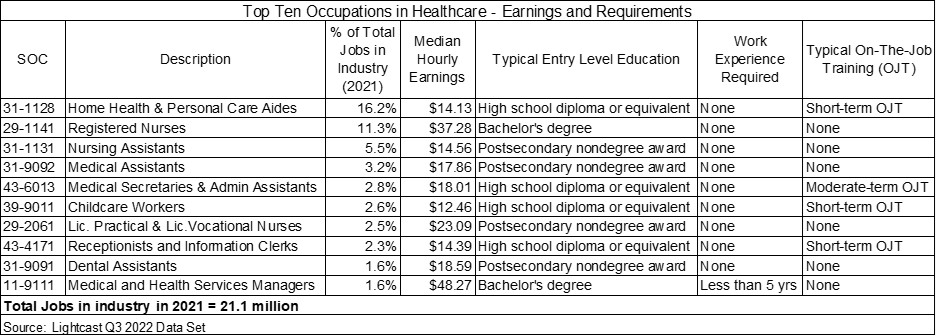 Many of the jobs typically requiring less than a bachelor’s degree are also relatively low paying, particularly those in home health and personal care, nursing assistants, and childcare. This is a challenge for employers in filling openings as well as a personal economic burden to employees. One response has been to increase wages; however, wage increases have not been significant enough to fill openings particularly given the rise in inflation and burnout and stress from COVID. From 2021 to 2022 wages in the healthcare industry grew 2.1%[4] and are projected to grow 1.3% annually through 2027.
Many of the jobs typically requiring less than a bachelor’s degree are also relatively low paying, particularly those in home health and personal care, nursing assistants, and childcare. This is a challenge for employers in filling openings as well as a personal economic burden to employees. One response has been to increase wages; however, wage increases have not been significant enough to fill openings particularly given the rise in inflation and burnout and stress from COVID. From 2021 to 2022 wages in the healthcare industry grew 2.1%[4] and are projected to grow 1.3% annually through 2027.
Taking a deeper look into these jobs and based on job posting data from September 2021 through September 2022 (data taken from actual posting of openings on job listing and recruitment sites) for Home Health and Personal Care Aides, Nursing Assistants, Orderlies, and Psychiatric Aides, demand for jobs increased and advertised wages increased as well. Advertised wages increased from $14.98 per hour in September 2021 to $16.09 per hour in September 2022. With COVID revealing how critical many of these jobs are to societal well-being and the fact that an aging population will demand more and more care, it is clear that more will need to be nationwide to provide a qualified labor force while providing livable wages.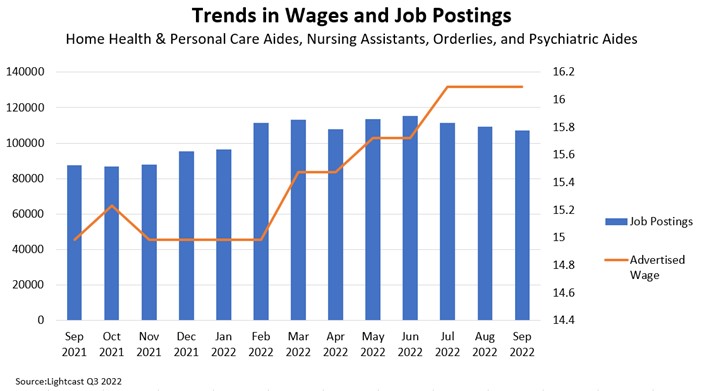 In preparing for what kinds of skills are critical job posting data further reveals that many of the jobs request skills typical of what you would expect in healthcare such as first aid, but many request human-centric skills including communications, compassion, and customer service.
In preparing for what kinds of skills are critical job posting data further reveals that many of the jobs request skills typical of what you would expect in healthcare such as first aid, but many request human-centric skills including communications, compassion, and customer service.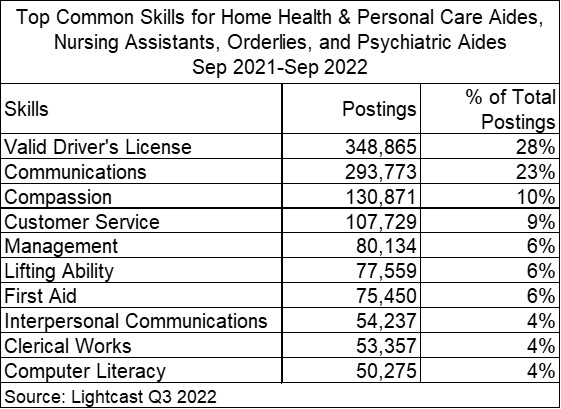
Looking Ahead: Healthcare and Business, Economic, and Workforce Development
Looking ahead, many of the factors that impact the economics of the healthcare industry are out of the control of economic and business developers at the regional and local levels, including federal regulation and spending, demographic trends, supply chains, and technological and scientific advancements. However, workforce development is a critical area where communities, regions, and states working together with industry education, and training partners can make an impact. The occupation data points to enormous opportunity for job creation and career development enabling further growth of the industry as well as greater prosperity. To achieve this requires a greater commitment to workforce development that considers recent and emerging trends in the labor force as well as emerging trends; working collaboratively among industry, education and training providers, and government; and a willingness to design new approaches that are worker-centric including providing greater access and opportunity for those traditionally left behind in economic growth. It requires not only raising wages so that those on the front line of care can make a decent living but also raising the overall capacity and value of the worker through relevant training and skills development designed to meet the workforce of today and into the future. It also means providing supporting services of housing, transportation, and family care and policies to support the long-term mental and emotional well-being of the worker. The following are current examples of how some of this is being done. The examples are centered around awareness and access, inclusiveness, adoption, and integration of digital technologies, and policy development.
The National Association of Counties (NACo) has made labor, employment, and workforce development a major focus of their work to support counties across the nation through policy research and advocacy. Recognizing the importance of workforce and in coordination with Workforce Development Month, they are highlighting investments counties have made using their ARPA funds to address critical workforce needs in care[5]. Cases include Erie County, NY, Maricopa County, AZ, Ramsey County, MN, Erie County, PA, and Hidalgo County, TX. All include funding to specifically increase access to healthcare jobs and careers and in particular nurses and front-line positions including entry-level assistant and technician positions. They also include efforts to recruit and provide access to these jobs by traditionally disadvantaged populations. Two are particularly worth noting in addressing the need for access:
Maricopa County Arizona has invested $14.5 million of its Recovery Funds into workforce development and job training programs. As part of this, the Banner Health Foundation received $1.24 million to expand the Career Pathways for Essential Frontline Healthcare Workers Program. Employees currently working in environmental services, culinary services, and patient transport positions are trained for in-demand skills and careers in healthcare with higher salaries, including medical assistants, certified nursing assistants, patient care assistants, technician roles in behavioral health, central sterile processing, pharmacy, and education. A focus is placed on educating and training employees who may not have graduated from high school due to access, language barriers, homelessness, or other socioeconomic factors[6].
Ramsey County Minnesota invested $1 million of its Recovery Funds in its Public Health Career Pathways Program to increase its public health workforce and give low-wage earners a pathway to careers as registered nurses or community health workers. Preference is given to applicants who live in Ramsey County, are single parents, receive public assistance, and/or are a member of an underrepresented group in the public health workforce. The program is comprehensive in that it addresses both education and support services to allow access. It provides college preparatory coaching and mentoring; reimbursement of tuition; expenses for transportation and/or childcare, wages to allow participants to enroll full-time; and paid work time to complete coursework[7]
How recruitment for jobs and careers is done by employers is a critical piece to creating greater awareness and access. In a recent article “Building the US Public Health Workforce Of The Future,” the authors highlight six strategies for addressing the healthcare workforce needs one of which is overhauling the recruitment process. “Public-health departments can capitalize on the opportunity to rebrand by launching modernized and innovative recruitment platforms that attract prospective hires. Such efforts can be digitally enabled and analytically driven, tracking talent gaps to inform recruiting and reducing turnaround times[8].” In their article, they also highlight the importance of creating awareness among those that are early in the education and career process and provide the example of the Public Health Foundation’s (HOSA) Future Health Professionals[9] which targets secondary and postsecondary students to introduce them to public health.
The Future Health Professional’s program is a fitting example of the need for new tools and digital technologies for workforce development. For this effort HOSA as partner shed with Tallo, which integrates digital platforms and community for “an end-to-end ecosystem of solutions for all phases of workforce and talent development[10]” Recognizing the critical role that technology and digitalization play in the future of healthcare, Massachusetts has created the Digital Innovation and Lifelong Learning program as part of its Healthcare Workforce Hubs[11]. These hubs connect MassHire Workforce Boards and community behavioral health employers to improve the skills and access to long-term careers for the incumbent and future workforce. They also focus on those who are particularly subject to barriers to employment. “Digital skills are a key component of a competent healthcare workforce. This is a statement that is true now and will be even more so going into the future. The Digital Innovation and Lifelong Learning program fills a void in the healthcare industry by teaching indispensable digital skills to entry-level, incumbent healthcare workers[12].”
Creating access to healthcare professions, including for those traditionally disadvantaged, has significant benefits for the workers and prospective workers as well as the healthcare industry and economy. In Building an Inclusive Economy Series – Strategies for Health-Care Workforce Development, the authors strongly make this case: “The health-care sector has an opportunity to make a profound social impact on surrounding communities while at the same time improving its bottom line. As the United States undergoes a rapid demographic shift, the nation’s healthcare sector is embracing this new diversity as a path that leads to shared economic growth and prosperity. The healthcare sector, along with business leaders, elected officials, and economic development strategists, is recognizing that increased diversity can lead to increased revenue and market share — if diverse groups can actively participate and contribute as workers, innovators, leaders, and entrepreneurs.[13]” The authors’ piece goes beyond theory and provides specific case studies and examples of actionable strategies that range from training, procurement, long-term career development, internships, internships, and more.
The above is meant to provide specific examples of workforce development in healthcare. It can be challenging and time-consuming to stay informed of new developments, particularly in an ever-changing workforce and economic environment. A great resource for staying informed is through the Next Generation of the Healthcare Workforce Learning Collaborative of the National Governor’s Association, particularly for state-wide initiatives. This provides a national clearinghouse of best practices[14].
Summing It Up: An Imperative for a Focus on Healthcare and Workforce Development
Healthcare is often overlooked in business, economic, and workforce development as practitioners and policymakers focus on other industries seen as being more valuable due to export potential or having higher wages. This is shortsighted. Think about healthcare businesses, organizations, and workers in your family, neighborhood, and community. What do they mean to you and the socio-economic well-being? They mean a job, a business, critical care for a family member or co-worker, an anchor to business and employment districts, and more. Now think if they did not exist. What businesses, families, and workers would be impacted? That is the crisis that many communities are facing particularly rural and underserved urban areas. Lack of critical workforce is a large factor in this problem and focused and informed policies, strategies, and actions can and are addressing this for the future.
_______________________________________________________________________________
[1] IBISWorld Industry Report 62 – Healthcare and Social Assistance in the US, September 2022
[2] Ibid
[3] Ibid
[4] Ibid
[5] www.naco.org/blog/workforce-development-month-arpa-investments-public-health-workforce
[6] www.bannerhealthfoundation.org/news-information/articles/banner-receives-1-million-from-maricopa-county-for-health-care-workforce-development
[7] www.ramseycounty.us/jobs/career-pathways-program
[8] Building The US Public Health Workforce Of The Future, Pooja Kumar, Emily Lurie, and Ramya Parthasarathy, McKinsey & Company, February 2022, www.mckinsey.com/industries/public-and-social-sector/our-insights/building-the-us-public-health-workforce-of-the-future
[11] https://commcorp.org/header_program/health-care-initiatives/
[12] Ibid
[13] Building an Inclusive Economy Series – Strategies for Health-Care Workforce Development, Kalima Rose, Mary Lee, and Victor Rubin, 2015 PolicyLink, www.policylink.org/sites/default/files/pl_brief_nola_healthcare_FINAL_0_0.pdf
[14] www.nga.org/projects/next-generation-of-the-healthcare-workforce-learning-collaborative/